General Principles of Antibiotic Stewardship
Approach to Prescribing
First, some definitions:
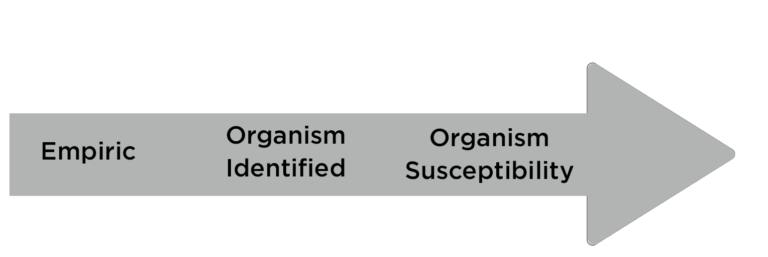
- Empiric prescribing is based on a syndrome without microbiology data to support a diagnosis
- Definitive prescribing is based on proven microbiology results that fit with the clinical diagnosis.
Clinical pearl: Always ask yourself when a test identifies an organism if that organism seems to be causing disease in the patient or is irrelevant?
Golden Rules of Antibiotic Prescribing:
- Know your host
- Name diagnosis as specifically as possible
- Get exposure history
- Know LOCAL antibiogram
- Name the bug THEN pick the drug
Ask yourself daily:
- Does patient have a bacterial infection?
- If an organism is identified, is it causing disease?
- What is the clinical diagnosis?
- Where is the infection located?
- Can I name the top 1-3 pathogens causing disease?
- What is the first calendar day of effective treatment?
- What is the last planned calendar day of treatment?
Antibiotic Spectrum
- Humans are colonized with normal, beneficial bacteria
- Ideally, antibiotics should only eliminate bacteria that are causing infection
- The antibiotic spectrum index gives you an idea of how “broad” the antibacterial is
- The higher the number, the “broader” the antibiotic
- The more “broad” an antibiotic is, the more normal bacterial colonizers will be affected outside of the targeted pathogen
- We want to use the “narrowest”, effective drug possible
Antibiogram
An antibiogram is a report that shows how susceptible strains of pathogens are to a variety of antibiotics in a given location.
It can help when creating local clinical protocols (e.g, what is the best treatment for urinary infections in our system) and also to get an idea of how likely the current regimen will be successful while you are waiting for full susceptibilties of an identified organism.
Finally, it can identify antibiotic resistance trends within a geographic area.
An antibiogram is not useful once full susceptibilities come back for a definitive pathogen. In that case, you should use susceptibilities of the pathogen of interest in that particular patient.
An antibiotic is a double-edged sword. With the benefits comes costs:
- Resistance (both for an individual patient and society)
- Disruption of pediatric microbiome
- Diarrhea
- Neutropenia
- Allergic or perceived allergic reaction
- C. difficile colitis (which can occur up to 90 days after treatment)
- Cost, discomfort to patient
Copyright © 2023 Georgia Pediatric Antibiotic Stewardship
